Hemorrhoids Frequently Asked Questions
Hemorrhoids are very common and oftentimes don’t present any threat, although the pain and discomfort can take a while to go away. If not treated, hemorrhoids can develop into something else more serious, not to mention the atrocious time you’ll have to try to live with the immense pain.
In this article, we answer the most searched questions about hemorrhoids, including their symptoms, if they can be confused with other diseases, what happens if you get hemorrhoids while pregnant, what they look like, and general tips to help you prevent them from bothering you.
1. Do Hemorrhoids Itch?
Hemorrhoids present itchiness, pain, and general discomfort for those who have them. To understand better why this happens, let’s take a look at what hemorrhoids are and how they can affect your body.
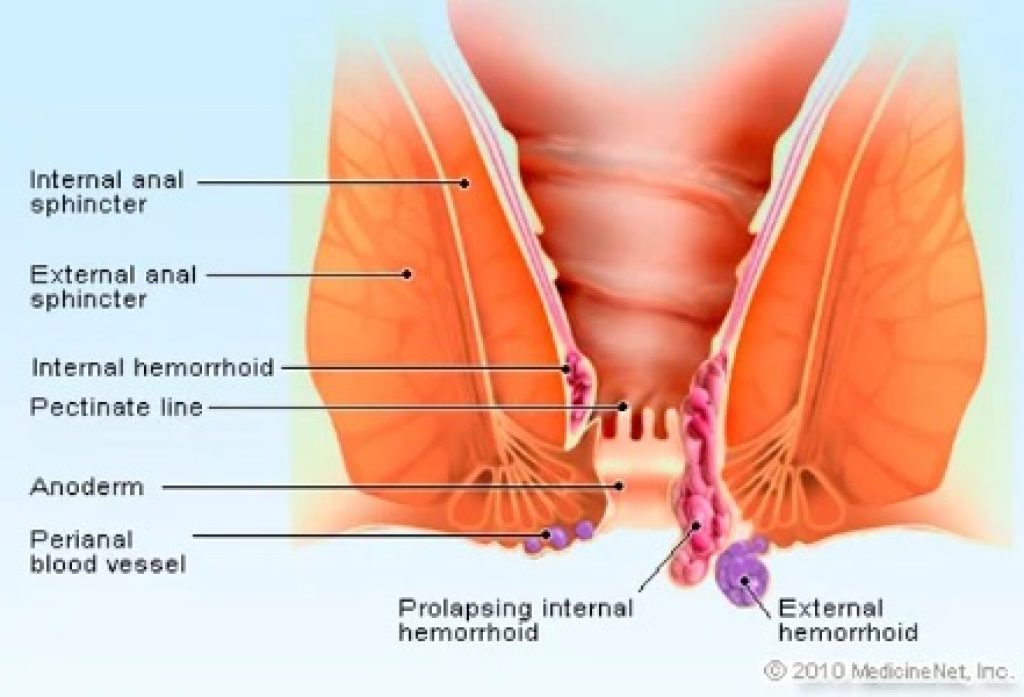
There are two types of hemorrhoids, external and internal. The first one can be found below the skin that surrounds the anus, whereas the second type is found inside the rectum. When straining while using the bathroom it can happen that an internal hemorrhoid is pushed until it exits the anus, causing a prolapsed internal hemorrhoid.
When this happens, hemorrhoid causes mucus to stick to the outer part of the anus skin, causing irritation and itching. If you leave this untreated, the pain, itchiness, and discomfort will continue.
1.1. Other Causes Of Anal Itching
If you notice anal itching, there may be a few possibilities why this is happening aside from hemorrhoids. Other causes of this include yeast infections, anal fissures, stool leakage, proctitis, sweat buildup, herpes, ringworm, scabies, genital warts, body lice, psoriasis, and cancer.
Poor hygiene can also lead to itchiness as well as over-cleaning the area since it can cause small tears and cracks (microscopical) and dry out skin due to the chemicals found in creams, cleansers, and wipes.
If you have any doubts about whether you have hemorrhoids or another condition, schedule an appointment with your doctor to get a precise diagnosis.
1.2. Avoiding Itchiness & Easing The Pain Of Hemorrhoids
To avoid anal itching, also known as pruritus ani, consider using plain white toilet paper and not scented varieties, as well as wearing loose clothing, wiping gently, wearing cotton underwear, and avoiding chemically-treated wipes.
If you’re looking to ease hemorrhoid itching, try not scratching since it can make the situation worse. Apart from this, have a good hygiene routine where you keep the area clean (allergen-free soap and water will do just fine) to avoid infections.
Some tips to stop itchiness are soaking in a bathtub, numbing the area with a cold press, and using a topical protectant.
2. Can Hemorrhoids Be Confused With Something Else/Worse?
The symptoms of hemorrhoids include pain, itchiness, discomfort while sitting or standing up, as well as bleeding. But people can sometimes think they have hemorrhoids when in reality they are suffering from a different condition. It is important that, if the symptoms do not go away on their own or with the help of medication after two weeks, you go to see a doctor immediately so they can rule out any other condition.
The most common diseases that share some of the symptoms of hemorrhoids are:
- Anal fissures. Small tears in the anal canal can cause pain, bleeding, and a burning sensation. They can appear at any age and are typically caused by constipation (1).
- Colon, rectal or anal cancer. It can appear with similar symptoms to hemorrhoids and is commonly accompanied by bleeding or a lump.
- Anal warts. Caused by HPV (human papillomavirus) and can result in bleeding and discomfort. If not treated, they’ll continue to grow and can increase the chances of getting anal cancer. According to the American Cancer Society, “people who have had anal warts are more likely to get anal cancer. This is because people who are infected with HPV subtypes that cause anal and genital warts are also more likely to be infected with HPV subtypes that cause anal cancer”.
3. Can You Get Hemorrhoids When Being Pregnant?
Yes, and in fact, pregnant women are more prone to getting hemorrhoids due to the uterus getting bigger and applying pressure on veins, causing them to swell and resulting in hemorrhoids.
Further, an increase in progesterone during this time is a major contributor to developing hemorrhoids since it relaxes the veins and makes them more likely to swell. An increment in your blood volume can also lead to hemorrhoids during pregnancy because it can also enlarge the veins. Other additional causes of hemorrhoids during pregnancy include straining from carrying extra pregnancy weight, straining during bowel movements, and sitting or standing for long periods of time.
Hemorrhoids are more likely to appear in pregnant women who suffer from constipation, and those who have to take pregnancy hormones can also experience hemorrhoids due to the medicine’s ability to slow down the flow of food in the digestive tract (1).
3.1. Preventing Hemorrhoids During Pregnancy
Not being constipated is the number one goal for staying away from hemorrhoids. To achieve this, try to incorporate more fiber-rich foods into your days like fruits, vegetables, and whole grains. Drink plenty of fluids to keep yourself hydrated and to allow your body to detox and go to the bathroom easily.
What’s more, don’t wait until you can’t hold going to the bathroom. As soon as you feel the need to because otherwise, you can make things a lot harder to get rid of. Try not to stay too long seated or standing up because it can put pressure on your rectal veins. Make sure you walk around from time to time to stay away from hemorrhoids.
4. How Do Hemorrhoids Look Like?
Internal hemorrhoids are protrusions from the anal canal or rectum wall. They can manifest as lumps or lengthy protrusions depending on their severity. As for external hemorrhoids, on and around the anus, they appear as one or several pimples. These are visible to you or a doctor from the outside.
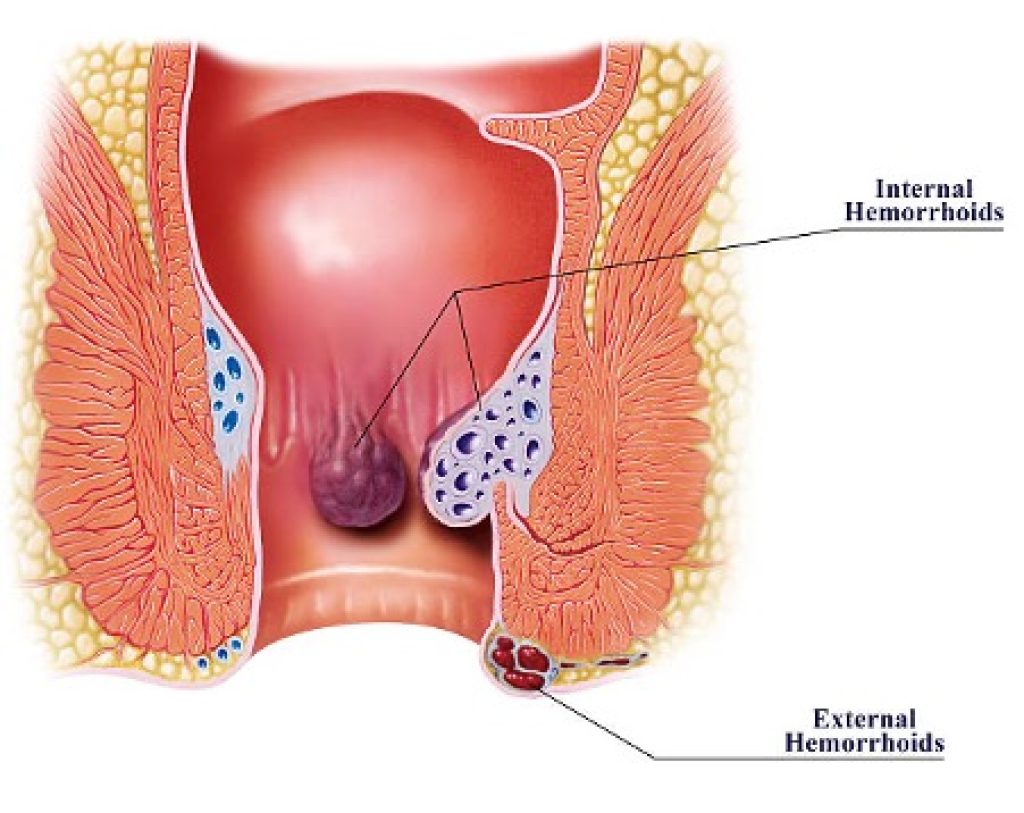
Prolapsed hemorrhoids look different depending on how serious the issue is. When you strain, less significant prolapsed hemorrhoids emerge from the anus, but when you relax, they automatically retract. More severe prolapsed hemorrhoids, however, continue to protrude from the anus.
5. Can Hemorrhoids Pop Or Burst?
Hemorrhoids can burst, but they cannot pop like you pop a pimple since they are very different from the latter. Since hemorrhoids are swollen rectal veins, the only time where they can burst is to secrete blood but only in the most severe cases of hemorrhoids.
If you’re wondering when a hemorrhoid can burst, it will do so on its own in situations when hemorrhoids have become thrombosed (bulging and causing a lot of pain). It will begin to bleed if it can’t hold the blood inside the vein, but the reality is that it may be a bit difficult for this to happen, thus a thrombosed hemorrhoid causes a lot of pain and most people tend to go to the doctor to solve the issue.
5.1. Should I Try To Pop A Hemorrhoid?
Please do not try to pop hemorrhoids since it can make the issue worse. Go to the doctor to have an expert’s view on the problem and ask about ways to relieve the symptoms of hemorrhoids. If pain is unbearable or you have dizziness/fainting, seek emergency help as soon as possible.
A burst hemorrhoid can bleed for anywhere between a few seconds and a few minutes. A burst hemorrhoid shouldn’t bleed for longer than 10 minutes. Constipation will often make hemorrhoids worse, resulting in spotting and brief bursts of bleeding.
If hemorrhoid explodes, it’s a good idea to visit a doctor. At that point, it normally doesn’t require considerable treatment, but it’s still a good idea to get the region examined to be sure nothing more severe is going on. If you’re seeking pain relief and infection prevention, a sitz bath is a wonderful idea.
6. Can Hemorrhoids Cause Constipation?
Constipation is the infrequent, possibly hard, dry, and painful passage of stools. There can be pressure on the rectum and a sense of incomplete evacuation. Colon distension can result in abdominal pain and a bloated feeling in the belly.
At least once every two to three days, you should have an easy-to-pass, moist-formed stool. Your chance of developing symptomatic, larger hemorrhoids will go down as a result. Less than two minutes should be spent on the toilet. There should be no straining.
Answering the title’s question, no, hemorrhoids are not the cause of constipation nor can they cause it if you have them. What can happen is that due to constipation, hemorrhoids can appear.
Constipation can be completely avoided if the correct quantity of fiber is consumed and by drinking enough water. Stress, consuming too much dairy, taking antacid medications, or even spending a lot of time sitting still are additional reasons for constipation. Because of this, it’s essential to keep active, consume foods high in fiber, and drink enough water. You should also avoid taking too many antacids. If you are aware that you are prone to hemorrhoids, attempt to cut back on your dairy consumption as well as stress.
7. How Do Hemorrhoids Heal?
Usually, hemorrhoids’ symptoms go away on their own, but depending on how severe they are a doctor may recommend a specific treatment plan.
By changing small habits in your life, such as incorporating more fiber in your diet (fruits, vegetables, whole grains) and not straining during bowel movements you can relieve hemorrhoid symptoms in 2-7 days. Further, drinking more water contributes to preventing hemorrhoids, and applying ice packs to the area works great for alleviating the pain.
If you require a more precise treatment, there are several over-the-counter medications you can choose from to get rid of hemorrhoids, itchiness, and swelling.
For cases that did not get better with home treatments or over-the-counter medications, surgery is an option.
7.1. Professional Treatment For Hemorrhoids
There are some minimally-invasive and surgical procedures for treating hemorrhoids. The first ones include sclerotherapy, rubber band ligation, and coagulation.
Sclerotherapy involves injecting a solution into internal hemorrhoids, which results in the formation of scar tissue. Hemorrhoids contract as a result of the disruption to the blood supply. Rubber band ligation is one of the most common treatments that doctors choose to use, in which a specific rubber band is wrapped around the hemorrhoid’s base to halt the blood flow, causing hemorrhoids to contract. Finally, coagulation applies electrical currents to internal hemorrhoids, which causes scar tissue to form and hemorrhoids to shrink.
As for surgical procedures, the most common ones are hemorrhoid stapling and hemorrhoidectomy. The first one requires a doctor to use a specific stapling instrument to remove internal hemorrhoid tissue from a prolapsing internal hemorrhoid. The second one is desired for removing big external hemorrhoids and prolapsing hemorrhoids that did not respond to other treatments and requires anesthesia.
Hemorrhoids FAQ Conclusion
This post aims to answer the most common questions about hemorrhoids. To sum up, hemorrhoids can be caused by different things such as constipation, sitting or standing for long periods, and more. They can cause pain and bleeding and usually go away on their own. Over-the-counter medication is available and, in case you do not feel better after two weeks, it is recommended that you visit your doctor.
If the pain becomes unbearable or you suffer from dizziness or faintness while having hemorrhoids/bleeding, seek emergency help. It is advised that the minute you notice any sign of bleeding talk to a doctor to ensure you’re treating the right problem with a specific solution.
To prevent developing hemorrhoids, try incorporating more fiber into your diet with fruits, whole grains, and vegetables. Drinking plenty of fluids and doing physical activity can also reduce the chances of this happening.